
Consumer and Provider Factors the Influence Readiness to Hearing Care Treatment
Amyn M. Amlani, PhD
Author’s Note: Positions of this paper were adapted from Amlani (in press).
Introduction
The consequences of untreated hearing loss in older consumers include a poorer quality of life (QoL) and loss of autonomy (Gopinath et al, 2012; Davis et al, 2016), and is associated with negative health conditions such as social isolation, depression, and reduced cognitive function (Livingston et al, 2017). For adults with hearing loss, hearing aids are the most common audiological rehabilitation intervention, improving the individual’s psychological, social, and emotional well-being (Laplante-Lévesque et al, 2010). Despite the benefits of hearing aids, uptake is often delayed, averaging between 7 and 10 years after the time that hearing difficulties were first revealed (Simpson et al, 2018). A by-product of this delay in seeking treatment is an increase in the average age of first-time hearing aid users to upwards of 70 years (Henshaw et al, 2012). Furthermore, consumers who receive treatment struggle with consistent daily use and long-term adherence (McCormack & Fortnum, 2013).
The ability to predict consumer readiness and acceptance towards treatment outcomes in hearing care has been evasive. Historically, health behavior models (e.g., Transtheoretical Model, Health Belief Model) have been used to quantify the psychosocial aspects of behaviors and attitudes related to hearing aid uptake and adherence. Recent research shows that these models lack sensitivity in quantifying intrinsic (e.g., attitudes, beliefs, intentions) and extrinsic (e.g., social, economic, environmental) factors that can affect perceptions towards hearing health (for a review, see Amlani, 2016, and Couslon et al, 2016). This paper provides the reader with an overview of various individual factors that have the potential to influence treatment readiness and acceptance from both the consumer and provider perspective.
 Consumer Readiness
Consumer Readiness
For consumers, readiness, or motivational engagement, is the concept of accepting a treatment intervention option with enthusiasm, optimism, and motivation (Erdman, 2000). Factors that influence the consumer’s perspective of readiness include:
- Self-perceived hearing loss
- Stigma
- Personality
- Health Literacy
 Self-Perceived Hearing Loss
Self-Perceived Hearing Loss
Self-perceived hearing loss is a factor that influences readiness towards treatment. In a retrospective study of >5000 responses reviewed from the US National Health and Nutrition Examination Survey (NHANES), roughly 1 in 4 respondents was found to have measurable hearing loss (Angara et al, 2021). Of this subgroup of respondents, only 1 in 6 (i) correctly identified their hearing status, and (ii) adopted hearing aids. In addition, results from MarkeTrak 10 indicate that self-perceived hearing loss increases as a function of severity of loss (Carr, 2020). Specifically, only 14% of individuals with self-reported mild hearing loss adopted traditional hearing aids, with adoption rates increasing to 37% and 58% for moderate and severe hearing losses, respectively.
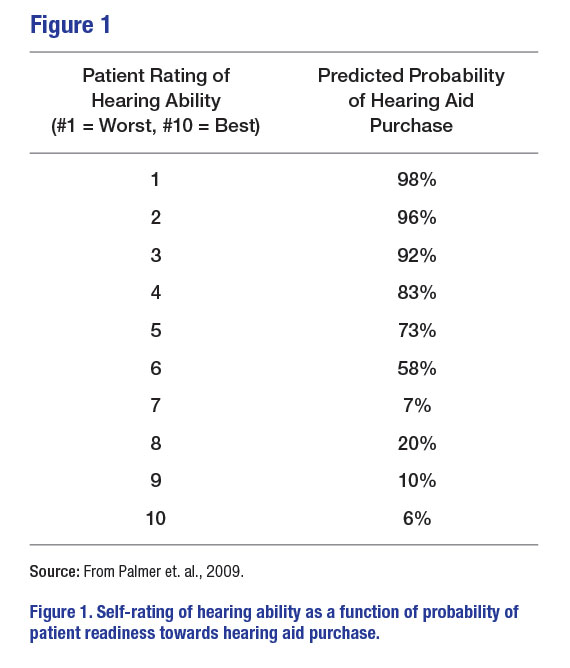
Clinically, audiometric threshold results are neither predictive of consumer self-perceived hearing handicap nor their readiness in obtaining amplification. Palmer and colleagues (2009) found that asking consumers the question, “How would you rate your overall hearing ability?” was a better predictor of assessing readiness towards amplification than hearing status. As seen in Figure 1, ratings between 1 and 5 have a high probability (i.e., > 70%) of predicting readiness towards hearing aid adoption, while scores of between 7 and 10 resulted in a slim probability (i.e., < 20%) of patient readiness towards hearing care services. Note that a rating of 6 has a near-chance probability (i.e., 58%) that the consumer is receiving help in overcoming their hearing difficulties.

Stigma
Stigma is the devaluation or discrimination towards an individual based on a distinguishing characteristic (Heatherton et al, 2000). In hearing care, stigma and agism are associated with wearing a hearing aid, and not necessarily the hearing loss itself. This perception, called the hearing aid effect, was first coined by Blood and colleagues (1978). With the increased use of consumer electronic products, such as Bluetooth receivers, earbuds, and earphones, one would presume a decline in the hearing aid effect. Rauterkus and Palmer (2013) evaluated the influence of various types of devices worn by young men and found no significant stigma associated with hearing aid use as perceived by non-hearing-aid-wearing young adults. However, there is little evidence, to date, on the diminished perception of the hearing aid effect towards consumer electronic products by neither those with selfperceived hearing loss seeking amplification strategies nor current users of hearing aid technology.
 Personality
Personality
Personality is the characteristic pattern of thoughts, feelings, and behaviors that are unique to everyone. Hearing loss— independent of severity—is known to influence psychological and social issues, with emotional and societal consequences (Cox et al, 2005). Gatehouse (1990), for example, found that factors such as personality and intelligence did not predict performance with hearing aids, but did predict self-perceived hearing difficulties.
A study conducted in Sweden evaluated several variables in a sample of 400 individuals aged 80-98 years over a six-year period. Of the variables tested—which included physical, mental, social, cognitive, and personality measures— individuals with hearing loss were found to have reduced extraversion (i.e., outgoing, optimistic personality) leading to increased social isolation (Berg & Johansson, 2013). These authors found that the lack of social interaction led to a change in personality through increased depression (i.e., neuroticism personality), with little or no changes in emotional stability.
Cox and colleagues (2005) evaluated the personalities of individuals pursuing hearing aids to determine whether pursuers’ personalities varied from the general population. Self-reported data were obtained from 230 older adults using a cross-sectional survey. Findings revealed:
- Individuals with neuroticism (i.e., having dispositions of anger, emotional instability, depression) were unlikely to seek hearing aids, a behavior consistent with a perception of devaluation (i.e., stigma).
- Individuals who were willing to learn new things tended not to seek hearing aids (i.e., openness personality type). Instead, these individuals were more inclined to rely on environmental variables to overcome their hearing difficulties.
- Individuals who are skeptical and suspicious (i.e., showing lack of agreeableness) were more inclined not to seek help in overcoming their hearing difficulties. For this personality, it is important that providers apply best practices that demonstrate value proposition in improving hearing health outcomes.
Health Literacy
Health literacy is defined as the degree to which an individual has the capacity to obtain, communicate, process, and understand health information and services to make appropriate health decisions (Somers & Mahadevan). There are examples of health literacy in hearing care. Wells and colleagues (2020) explored the characteristics associated with health literacy (i.e., limited versus adequate), medical costs, and medical gaps in a sample of 19,223 adults aged > 65 years who completed a health survey. Health literacy, hearing loss, and hearing aid use were assessed through self-reports. Results revealed that limited health literacy was associated with older age, male gender, lower income, poorer health conditions, and those with hearing loss who did not use hearing aids. Similarly, Tran et al (2020) assessed the association between health literacy and (i) degree of hearing loss, and (ii) hearing aid adoption in a sample of 1,376 consumers against demographic factors (e.g., age, gender, employment status, race, language) and insurance coverage. Findings revealed that consumers with low health literacy had an increased likelihood of presenting with higher degrees of hearing loss. Interestingly, those with lower health literacy were no less likely to obtain hearing aids compared to consumers with adequate health literacy.
Recent research has also assessed the consumer’s ability to manage a self-fit hearing aid through written instructions. Convery and colleagues (2017) asked participants and their partners—recruited from culturally diverse and linguistic backgrounds—to assemble a pair of self-fit hearing aids using culturally and literacy appropriate written instructions and illustrations. Results revealed that study participants could manage the self-fitting hearing-aid assembly successfully. In another study, Convery et al (2017) evaluated the ability of a group of adult participants—without and with hearing aid experience—to setup a pair of selffitting hearings for their own use. Participants were provided the product’s accompanying written and illustrated instructions to complete the task, with optional assistance from a lay partner. Results revealed that just over 50% of participants—independent of their experience with hearing aids—were able to perform the self-fitting procedure successfully. These authors conclude that participants’ performance, in part, could have been influenced by the instruction set and physical design of the self-fit hearing aid, both of which would benefit from refinement.
 Provider Readiness
Provider Readiness
Provider readiness is the extent to which supply-side stakeholders provide services and products that meet consumers’ needs. Factors that influence provider readiness include:
- Clinical Bias
- Patient-Centered Care
Clinical Bias
Glaser and Traynor (2017) report that provider readiness is often biased and partial to the characteristics of hearing loss, audiometric test results, and an assumption of how hearing loss is impacting the consumer. As a result, providers fail to meet consumer expectations. This finding was recently confirmed by Amlani (2020), who found that service delivery expectations for an in-person hearing evaluation and possible rehabilitative treatment intervention were unmet postappointment on several dimensions (e.g., trust, empathy, shared decision-making, communication) for consumers with untreated, self-perceived hearing loss.
 Another supply-side consideration that influences consumer readiness is the stereotype that Baby Boomers’ hearing sensitivity is more severe than individuals from the Silent generation because of recreational noise exposure. Research, in fact, indicates the reverse, where Baby Boomers hearing difficulties are less severe than anticipated because of improvements in occupational standards and nutrition compared to individuals from the Silent generation (Kochkin, 2012; Pacala & Yueh, 2012). In addition, patient readiness is hindered, in part, by clinical nomenclature such as mild and hearing loss, which negatively impacts consumer behavior towards hearing healthcare services (Alcock, 2014). Clearly, provider knowledge toward various service delivery offerings and their interactions with consumers markedly influence delivery and acceptance of hearing care services and products.
Another supply-side consideration that influences consumer readiness is the stereotype that Baby Boomers’ hearing sensitivity is more severe than individuals from the Silent generation because of recreational noise exposure. Research, in fact, indicates the reverse, where Baby Boomers hearing difficulties are less severe than anticipated because of improvements in occupational standards and nutrition compared to individuals from the Silent generation (Kochkin, 2012; Pacala & Yueh, 2012). In addition, patient readiness is hindered, in part, by clinical nomenclature such as mild and hearing loss, which negatively impacts consumer behavior towards hearing healthcare services (Alcock, 2014). Clearly, provider knowledge toward various service delivery offerings and their interactions with consumers markedly influence delivery and acceptance of hearing care services and products.
Patient-Centered Care
Patient-centered care (PCC) is defined as the provision of care that is respectful of, and responsive to, an individual’s preference, needs, and values, and ensures that consumer values guide clinical decisions (Institute of Medicine, 2001). The literature indicates that most hearing care providers have not fully embraced PCC in their daily clinical interactions, as evidenced by (1) an absence of relationship-building with their patients (Grenness et al, 2015) (2) a lack of empathy when patients present psychosocial concerns expressed with a negative emotional stance (Grenness et al, 2015; Ekberg et al, 2014), (3) failing to include family member input as part of the treatment and management process of patient healthcare (Ekberg et al, 2015), (4) failing to acknowledge consumer’s emotional responses during the decision-making process with respect to hearing aid cost options (Ekberg et al, 2017), and (5) not promoting an equal opportunity for consumers to participate actively in their own treatment and management of their hearing impairment (Grenness et al, 2015).
Conclusion
Readiness is and will continue to be a key factor to improving hearing care service delivery, especially in the face of the consumer self-care segment. Providers must move beyond the use of audiometric threshold results when predicting hearing handicap and consumer readiness, as traditional clinical measures fail to highlight factors that adversely affect a consumer’s decision towards treatment intervention. As consumer readiness increases, so will hearing care service and product consumption.
In addition, demand towards hearing care treatment is correlated with stigma and personality. Specifically, there is a clear need by providers to understand the thoughts, feelings, and behaviors of consumers as they evaluate whether to pursue hearing care interventions. While the author is unaware of a single clinical inventory to assess consumer personality in impaired listeners, research is underway in the area of ambivalence—defined as a psychological conflict between opposing alternatives—and personal style. The objective of this research is to sensitize the provider to the consumer’s behavior and provide appropriate counselling strategies that have the potential to lessen barriers to treatment (Citron et al, 2022).
Lastly, health literacy—another aspect of readiness—will play an important role in whether demand increases, especially for alternative service models. Providers must be diligent in the creation of instructions and illustrations for self-directed services and self-fit products by ensuring that information is educationally and culturally appropriate for the intended user. For services provided either in person or virtually, providers should refrain from using professional and technical jargon, instead delivering evidence-based information, in lay terms, that promotes how a treatment has the potential to improve QoL. ■
References
- Alcock C. Trigger happy hearing: Using social triggers to promote regular hearing checks. Audiol Prac 2014;6(2):8-15.
- Amlani AM. Application of the Consumer Decision-Making Model to hearing aid adoption in first-time users. Sem Hear 2016;37:103-119.
- Amlani AM. Influence of provider interaction on patient’s readiness towards audiological services and technology. J Am Acad Audiol 2020;31(5):342-353.
- Amlani AM. Effect of determinants of health on hearing care framework: An economic perspective. Sem Hear In press.
- Angara P, Tsang DC, Hoffer ME, et al. Self-perceived hearing status creates an unrealized barrier to hearing healthcare utilization. Laryngoscope 2021;131: E289-E295.
- Berg AI, Johansson B. Personality change in the oldest-old: Is it a matter of compromised health and functioning? J Pers 2013;82(1): https://doi.org/10.1111/jopy.12030
- Blood GW, Blood IM, Danhauer JL. Listeners’ impressions of normal-hearing and hearing-impaired children. J Comm Dis 1978;11:513-518.
- Carr K. 20Q: Consumer insights on hearing aids, PSAPs, OTC devices, and more from MarkeTrak 10. Audiology Online. 2020: Article 26648.
- Available at: https://www.audiologyonline.com/articles/20q-understanding-today-s-consumers-26648. Accessed on 14 August 2022.
- Citron D III, Traynor R, Bray V, et al. Patient engagement: Learn personal styles & integrate motivational interviewing. 2021 Hamilton Captel:1-8.
- Coulson NS, Ferguson MA, Henshaw H, et al. Applying theories of health behavior and change to hearing health research: Time for a new approach. Int J Audiol 2016:55(S3):S99-S105.
- Cox RM, Alexander GC, Gray GA. Who wants a hearing aid? Personality profiles of hearing aid seekers. Ear Hear 2005;26(1):12-26.
- Davis A, McMahon CM, Pichora-Fuller KM, et al. Aging and hearing health: The life-course approach. Gerontologist 2016;56(Suppl 2):S256-S267.
- Ekberg K, Grenness C, Hickson L. Addressing patients’ psychosocial concerns regarding hearing aids within audiology appointment for older adults. Am J Audiol 2014;23(3):337-350.
- Ekberg K, Meyer C, Scarinci N, et al. Family member involvement in audiology appointments with older people with hearing impairment. Int J Audiol 2015:54(2):70-76.
- Ekberg K, Barr C, Hickson L. Difficult conversations: Talking about cost in audiology consultations with older adults. Int J Audiol 2017;56(11):854-861.
- Gatehouse S. The role of non-auditory factors in measured and self-reported disability. Acta Otolaryngol Suppl 1990;476:249-256.
- Gopinath B, Hickson L, Schneider J, et al. Hearing-impaired adults are at increased risk of experiencing emotional distress and social engagement restrictions five years later. Age Ageing 2012;41:618-623.
- Grenness C, Hickson L, Laplante-Lévesque A, et al. (2015). The nature of communication throughout diagnosis and management planning in initial audiologic rehabilitation consultations. J Am Acad Audiol. 2015;26(1):36-50.
- Heatherton TF, Kleck RE, Hebl MR, et al, eds. The Social Psychology of Stigma. New York: NY. The Gulliford Press. 2000.
- Henshaw H, Clark DPA, Kang s, et al. Computer skills and internet use in adults aged 50-74 years: Influence of hearing difficulties. J Med Internet Res 2012;14(4):e113. doi: 10.2196/jmir.2036
- Kochkin S. MarkeTrak VIII: The key influencing factors in hearing aid purchase intent. Hear Rev 2012;19(3):12-25.
- Laplante-Lévesque A, Hickson L, Worrall L. Rehabilitation of older adults with hearing impairment: A critical review. J Aging Health 2010;22:143-153.
- Livingston G, Sommerlad A, Ortega V, et al. Dementia prevention, intervention, and care. Lancet 2017;390:2673-2734.
- McCormack A, Fortnum H. Why do people fitted with hearing aids not wear them? Int J Audiol 2013;52:360-368.
- Pacala JT, Yueh B. Hearing deficits in the older patient: I didn’t notice anything. J Am Med Assoc 2012;307(11):1185-1194.
- Palmer CV, Solodar HS, Hurley WR, et al. Self-perception of hearing ability as a strong predictor of hearing aid purchase. J Am Acad Audiol 2009;20(6):341-347.
- Rauterkus EP, Palmer CV. The hearing aid effect in 2013. J Am Acad Audiol 2014:25(9):893-903.
- Simpson AN, Matthews LJ, Cassarly C, et al. Time from hearing aid candidacy to hearing aid adoption: A longitudinal cohort study. Ear Hear 2019;40(3):468-476.
