
Healthy Connections: An Educational Grassroots Marketing Odyssey
Bruce Essman
It goes without saying that audiologists are subject matter experts on all things hearing loss and hearing aid related. It is difficult, however, to put that expertise into action by systematically educating patients and the broader community of the value of health and wellness. This tutorial, as told through the odyssey of one practice, demonstrates how the core belief that educationally empowering patients with trusted advice is an ethical way to achieve business outcomes.
A Career Changing Epiphany
When growing up in a rural area, Janet Williams struggled to talk with her grandfather. Far too often, due to his severe hearing loss, conversational attempts were extremely frustrating. While suffering from vision loss and diabetes, he did enjoy tidbits of family dialogue that could be understood. Over the years, to her dismay, heartfelt talks and meaningful engagement became scarce. While his declining communication ability and quality of life difficulties were sad to see, it ultimately inspired her to select audiology as a career. She decided that being of service to those with chronic hearing challenges would be her professional mission.
Throughout her academic training, technical skills were paramount and with intellectual curiosity, she learned rapidly. During this rigorous process, she often thought about her hometown’s family physician who had strongly encouraged her grandfather to see a “hearing doctor” in the big city one hundred miles away, and how that compassionate audiologist brought precious sounds to life in his golden years. In retrospect, it was those clinicians’ combined expertise that empowered Grandpa Dave to actively participate in family celebrations that now were just fond memories.
Following formal training, Janet joined a busy ENT practice in the nearby big city. Although the reputable hearing doctor had retired, aggressive retail outlets now marketed what each claimed were the best hearing aids for the lowest prices. Finding the plethora of cost-focused ads confusing, she could not imagine how wary consumers could parse through contradictory claims. While being in a medical practice felt somewhat insulated from bewildering advertisements, in contrast, she observed the valuable continuity of her MD colleagues’ referral relationships with local primary care physicians. While Whole-person care concepts were often mentioned, seeing them in practice presented valuable lessons.
While clinical duties were rewarding, she was enamored with community outreach. Given their practice’s steady patient flow, while difficult to take on this pivotal role, she was motivated to bridge the interdisciplinary gap with current and prospective collaborators. With many primary care doctors as referral sources, she was surprised to ascertain, after so many years, few specialists knew about their ENT service lines, especially audiology. Encountering this awareness deficit, she was determined to more effectively spread the word about why and how Better Hearing is Better Healthcare.
In preparation to optimize external initiatives, she assessed baseline efficacy of the internal referral process between her ENT and Audiology colleagues. This was frequently a contentious point, as many patients requiring comprehensive evaluations were, despite challenges, hearing and understanding surgical instructions, either not recognized as needing help or sent to a Big-box store. While this delicate issue was raised during quarterly practice meetings, it never achieved priority status and systemic change was minimal. From Janet’s perspective, in contrast to their practice’s oft-expressed guiding principles, this underutilization of their collective expertise negatively impacted standards of care. By analogy, despite the diagnosis of these concerns being consistently validated, there was no dedicated team effort to successfully treat internal referral protocols. In contemplating opportunities to lead by positive example, she pondered what action steps actualize prosperity.
Facing internal barriers, she renewed external efforts to represent their practice. Lacking formal training in community outreach, intuition was her constant guide, including intent focus on raising awareness about how hearing loss related to not only aging, but various medical conditions such as dementia, the risk of falls, ototoxicity, diabetes, depression, and tinnitus. To her surprise, few healthcare collaborators knew about these comorbidities, as amid time-pressed schedules, discussion of them was outside their usual scope of practice. Despite real world concerns, she felt a sense of urgency to spread the word.
When seeking counsel from highly regarded audiologists nationally, a consistent theme was to intently study peer-reviewed literature on health literacy concepts, constructive challenges, and educational imperatives. In diligent research, this definition from the World Health Organization came to light:
“Health literacy implies the achievement of a level of knowledge, personal skills, and confidence to take action to improve personal and community health by changing personal lifestyles and living conditions. Thus, health literacy means more than being able to read pamphlets and make appointments. By improving people’s access to health information, and their capacity to use it effectively, health literacy is critical to empowerment.”
Further, “Meeting the health literacy needs of the most disadvantaged and marginalized societies will particularly accelerate progress in reducing inequities in health and beyond. Efforts to raise health literacy will be crucial in whether the social, economic, and environmental ambitions of the 2030 Agenda for Sustainable Development are fully realized.”1
Striking her as a career-changing epiphany, she felt highly motivated to accomplish patient-centric goals and less alone in her viewpoint.
Bumps in the Road
For the next year, Janet adeptly managed growth in her patient census and community outreach initiatives, applying educational acumen with both vital endeavors. As she tried sharing reputable information which emboldened patients to make better, more informed decisions, the inherent hurdles of achieving comorbidity awareness goals became clear. While, as a consumer, she saw retail stores cross-merchandise items with natural adjacencies, like computers and accessories or wine and cheese, busy healthcare providers did not methodically integrate cross-educational goals into clinical protocols. If you cannot improve what is not measured, what metrics would motivate and reward subject matter experts striving to demonstrate whole person care leadership?
As with many attempted innovations, momentum resembled an emotional roller coaster. Her lows were dominated by resistance within her own practice, along with many primary care clinics she visited. Internally, her colleagues, fully occupied by diagnostic testing loads, resented community outreach focus, thinking scarce time was being wasted. Although demonstrating little interest in developing relationships with potential referral sources, they collectively voiced skepticism about the worth of her initiatives. Notably, as external referrals increased, her fellow audiologists appeared surprised as to their origins. While disappointing on multiple levels, Janet learned invention required tenacity.
In community, while genuinely advocating for patient-centrism, rude awakenings were constant. Being well-prepared for each primary care office visit was her fervent discipline. Even with the power of a positive attitude, those she encountered expected a sales pitch, not medical discussions about hearing-related quality of life goals. After numerous uncomfortable interactions, she contemplated how to, within a few moments, distinguish her interdisciplinary education role from that of pharmaceutical reps “talking product”. With health literacy goals near and dear, she was eager to tell them something, not sell them something.
Her highs were meeting like-minded professionals with an affinity for comorbidity education, who avidly sought peer-reviewed research relevant to patients entrusted in their care. One success story was of a devoted physician’s assistant, who enthusiastically engaged. Playing a key role in a bustling primary care practice where comorbidity diagnoses were prevalent, she recognized hearing loss related to many of them. Further, in the course of observing clinical dialogue, she was acutely aware of patients unable to comprehend verbal instructions. Prompted by her collaborative spirit, Janet shared a fascinating article on “The impact of health literacy on patient understanding of counseling and education materials.”
In part it read, “All world health organizations would likely agree that access to information starts with being able to hear it, ask questions and understand the responses. In this regard, hearing-impaired patients are at a disadvantage. Clear communication is critical to hearing-impaired patients’ overall healthcare, making it even more important that hearing-impaired patients can easily access direct counseling and supplemental information. Clear communication via functioning amplification and utilization of good listening strategies can provide better access to information from all healthcare professionals. Without clear communication, it is likely that hearing-impaired patients will not become successful users of the healthcare system. It is eminent that audiologists communicate with their patients about their hearing healthcare because not only does it increase the likelihood, they will both be more satisfied with their hearing healthcare and more satisfied with their overall healthcare. In this regard, audiologists are a critical link to World Health Organization’s (WHO) goal of improving health literacy for patients.”2
As patient-centered discussions with the physician’s assistant flourished, they spoke about specific cases such as an elderly gentleman, who reminded Janet of her grandfather. Sadly, like Grandpa Dave, he struggled to see well, with advanced glaucoma having taken its toll. In addition, heart disease limited stamina and balance issues were apparent. Amid a recent visit, the physician’s assistant observed his frustration with inability to converse effectively. With that behavioral prompt, she referred to Janet, who, based on thorough evaluation, fit, and trained him on advanced hearing aids, along with suggesting using a pocket talker at his doctor’s appointments. Joys of hearing were rediscovered, and he was all smiles at a family wedding celebration. During those emotional moments, his pleasure spoke volumes and at a subsequent follow-up appointment, memorable pictures were happily shared.
A Welcome Spirit Arrives
As time went by, Janet diligently honed her skills at the ENT practice, although the lack of bona fide support for her educationally focused outreach initiatives persisted. Being intensely loyal, she grappled with clear disconnects between her aspirations and those of colleagues, at later career stages, who were contentedly set in their ways. Daily cues indicated that, from a career perspective, this position was not ideally fit, and as with her patients’ decisions about quality-of-life issues, she recognized crucial choices were inevitable. Enduring constant deterrents, she was unsure where pathways forward might lead. Fortuitously, she received a call from her hometown family physician whom she had not spoken with for many years. Dr. Carter was an admired medical leader in their local community, now a rapidly growing retirement destination. Case in point, the regional hospital’s expansion persuaded more primary care providers and specialists to establish practices, gratifying residents seeking expert care nearby. As the census increased, particularly among seniors, so did demand for interdisciplinary healthcare services.
Dr. Carter explained how a strategic alliance was formed between the hospital, local healthcare leaders and numerous senior living communities to promote her beloved hometown as an appealing choice for medical professionals seeking big city alternatives. At a recent meeting, assessments of current and prospective supply/demand status for various medical specialists were reported. The intention was to identify service gaps and make connections with trusted providers who might be interested in relocating. Remarkably they realized that, in order to take care of their expanding elder population there were geriatricians, ophthalmologists, neurologists, physical therapists and psychologists, but no audiologists, either at the hospital or in private practice. As discussions evolved about potential action steps, multiple participants advocated on Janet’s behalf, knowing of, in addition to hometown roots, her extensive training, stellar reputation and passion for interdisciplinary collaboration. Dr. Carter asked Janet if she had considered moving back home and starting her own practice, to which the answer was no. They agreed to speak again soon, as understandably, there were many implications, personally and professionally.
In the following weeks, Janet’s due diligence accelerated. Her parents were active seniors in their 70’s, and while fully supportive of whatever decision was made, were elated about her potential relocation. They were proud of her early career achievements and confident her compassionate style would delight many of their good neighbors. In poignant conversations, they talked about how Grandpa Dave inspired her exploring rewarding pathways in a clinical field now so near and dear.
At the ENT practice, status quo prevailed. Curiously, during community outreach visits, she began wondering how qualitatively better things might be if representing her own practice, in a place truly called home. Weighing the alternatives, Janet got back to basics in rediscovering The Why in her passion for audiologically-focused community outreach. With a steady flow of reputable evidence about how hearing loss relates to many medical conditions, it was continually alarming to realize how few were aware. While diagnosing and treating patients daily, and motivating their healthy choices, Janet felt refreshed ambition to play an influential role in elevating the profession. With educational needs chronic, these responsibilities were imperative. Who would actively inform more healthcare providers, patients, and families to be “in the know” …?
To put a finer point on it, perhaps triggered by the COVID19 epidemic, the term comorbidity, seemed better understood in both clinical and layperson dialogue. From a health literacy vantage point, this familiarity trend was now more of a tailwind than headwind. While public health policy had effectively conveyed the link between smoking and lung cancer, for example, what percentage of residents at senior living communities understood how hearing loss related to dementia, vision loss or the risk of falls? In her opinion, far too few, negatively impacting their quality of life, while substantially increasing systemic medical costs. As she counseled her patients on the benefits of healthy hearing, Janet concluded her career trajectory could reach new heights if, driven by the highest integrity standards, progressive visions could be actualized. With vigor, a follow-up call was scheduled with Dr. Carter, reviving a level of enthusiasm which, evidently, had been on extended leave. She sensed lifechanging decisions loomed large.
With great anticipation, their pivotal call took place. As expected, they talked in depth about career crossroads, specific opportunities, and prospective action steps. Dr. Carter was generous with advice and welcoming in spirit, constructively challenging Janet about her commitment to major changes. In that moment, she began realizing what a beneficial catalyst it would be to go from intense frustration with current circumstances to a new scenario characterized by a greater internal locus of control. Her destiny was her choice and when she said “Yes,” their mutual thrill was profound.
Creating the Plan
In a decisive manner, Janet gathered thoughts and documented plans. She immediately advised the ENT practice of her move, ensuring adequate time for necessary transitions. Trusted colleagues recommended that, particularly as they impacted patient care, sensitive changes be proactively and professionally coordinated. On a parallel track, with valuable support from Dr. Carter and the medical alliance’s support team, her new practice, Hometown Audiology, would open mid-November, just in time for the holiday season’s Gifts of Hearing. Beyond financial and administrative mechanics of clinic establishment, she avidly pursued networking opportunities with other medical providers associated with hospital systems. To facilitate this introductory phase, she was invited to join the monthly Doctors’ meeting over which Dr. Carter presided. With dozens in attendance, their warm welcome was an exhilarating experience that highlighted collaborative potential and allayed near term fears. She was not alone, which was incredibly gratifying.
 In talking to leading audiologists who had opened new practices elsewhere, she inquired about their grassroots educational marketing strategies and tactics. Broadly speaking, they advised logically mapping out patients’ journeys to well-informed decisions and a targeted trio focused on:
In talking to leading audiologists who had opened new practices elsewhere, she inquired about their grassroots educational marketing strategies and tactics. Broadly speaking, they advised logically mapping out patients’ journeys to well-informed decisions and a targeted trio focused on:
- In Practice
- In Community
- Online
Regarding In Practice factors, she was encouraged to first investigate outside of healthcare, at an Apple store and regional shopping mall, to immerse her mindset in the look and feel of their consumer merchandising. Aesthetics, visual clarity and streamlined flow were hallmarks. After all, a lot of high-priced talent and expertise was on display to study. Next, she got inside views of various practices within their local medical system. Contrasts were dramatic as some clinics appeared impressive, informative, and engaging, while others were less than stellar. Throughout this brainstorming process, she also received pictures and videos from industry colleagues who shared attractive layouts and this conceptual reference:
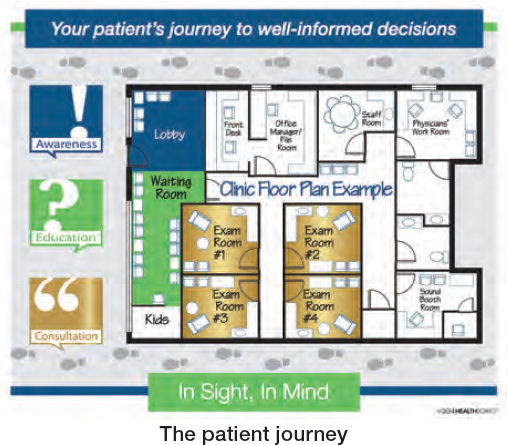 With valuable inputs, a detailed floorplan and new branding, Janet’s display plans began taking shape. With comorbidity awareness as a primary goal, she discovered a strategic concept known as Educate Well Monthly. With this framework, topics were aligned with national health observances such as, in addition to May being Better Hearing & Speech Month, this calendar:
With valuable inputs, a detailed floorplan and new branding, Janet’s display plans began taking shape. With comorbidity awareness as a primary goal, she discovered a strategic concept known as Educate Well Monthly. With this framework, topics were aligned with national health observances such as, in addition to May being Better Hearing & Speech Month, this calendar:
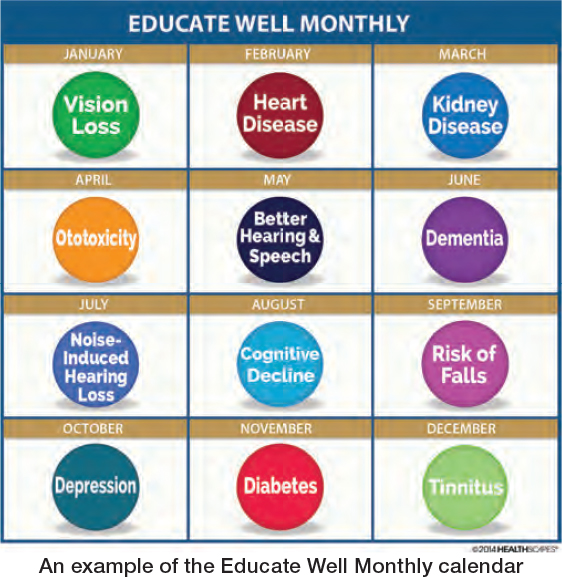 With various tasks to juggle related to her practice’s launch, this structured approach became the core of her Better Hearing is Better Healthcare educational initiatives. Instead of constant anguish about what to do next, systemic methods consistent with her high integrity guiding principles would lead the way. With this mission and vision, she walked through her clinical space, challenging herself to see and experience it from the patients’ view. From reception to testing and consult to checkout, she aimed to reverse engineer visual triggers and verbal communication processes. What was In Sight would be In Mind.
With various tasks to juggle related to her practice’s launch, this structured approach became the core of her Better Hearing is Better Healthcare educational initiatives. Instead of constant anguish about what to do next, systemic methods consistent with her high integrity guiding principles would lead the way. With this mission and vision, she walked through her clinical space, challenging herself to see and experience it from the patients’ view. From reception to testing and consult to checkout, she aimed to reverse engineer visual triggers and verbal communication processes. What was In Sight would be In Mind.
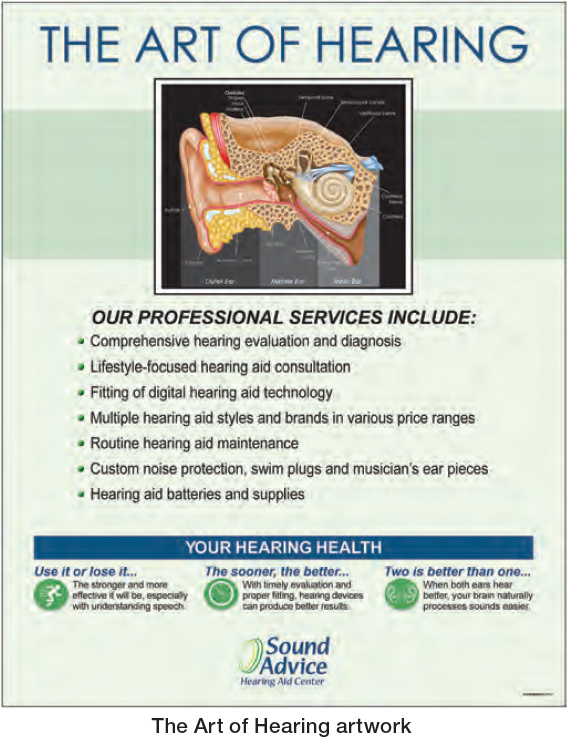

Her proprietary designs would emphasize research-based content which was patient friendly, and practice branded. In reception area, an upscale Art of Hearing™ canvas artwork design would proactively convey scope of practice. With various service lines to expertly provide, this eye-catcher would boost awareness and prompt evaluative inquiries. Nearby, a Hearing Health Education Center would be strategically placed.
When patients checked in, informative handouts would make relevant learning readily accessible. With intuitively paired backs, appealing documents would practically drive messages home, facilitating retention and discussion with loved ones. In addition, patients could become educational advocates with others in their circle of life, such as those challenged by hearing and vision loss who struggled with activities of daily living.
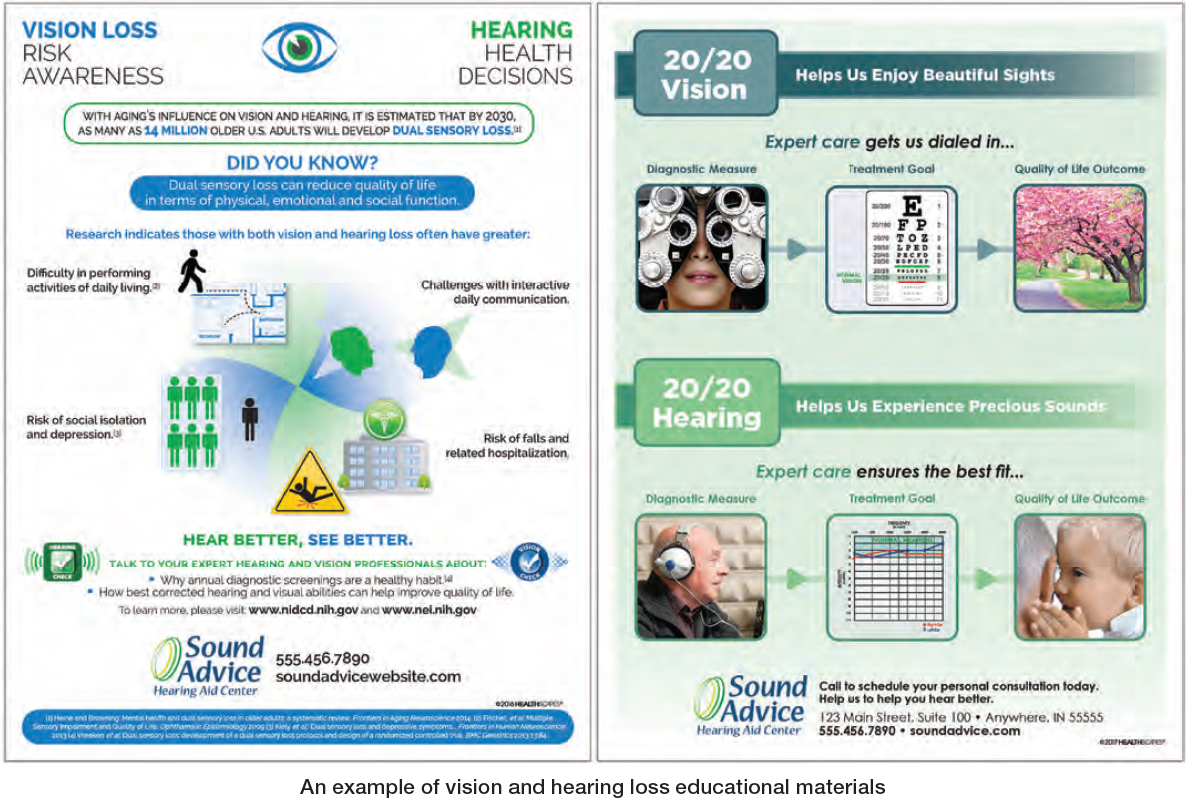
As patients journeyed through their clinical experience, other professional-looking designs would be viewed. From what Janet heard, this Did You Know? canvas artwork design was ideally placed in a consult location. With daily use in mind, this Talk Triad setting made sense. In Practice, Wellness Referrals mattered.
 True to her Whole Person Care passions and with networking effect goals integral, In Community was a foundational growth strategy. To plan accordingly, the medical system provided a contact list segmented by:
True to her Whole Person Care passions and with networking effect goals integral, In Community was a foundational growth strategy. To plan accordingly, the medical system provided a contact list segmented by:
- Generalists – primary care, internal medicine, and geriatricians
- Specialists including ENT, ophthalmologists, optometrists, cardiologists, nephrologists, oncologists, neurologists, physical therapists, psychologists, and endocrinologists
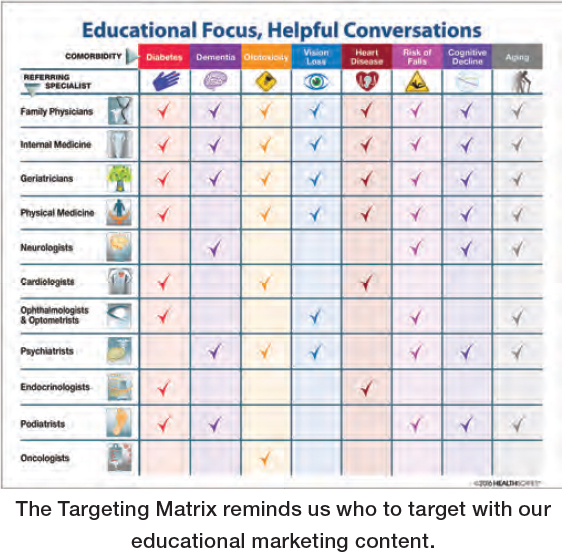
With the benefit of these profiles, she could easily “connect the dots” between Educate Well Monthly topics and specific care providers whose patient census had related medical conditions. This targeting construct was particularly useful:
Looking ahead to the new year, January’s focus was Vision Loss, aligned with Glaucoma Awareness Month. As Janet knew through her networking efforts, too few of her colleagues were aware of vision loss prevalence and the proactive testing necessary to detect the early stages of it.3
 By reviewing the medical system’s list and asking her own patients who provided their vision care, Janet identified multiple Ophthalmologists and Optometrists in close proximity. Just as helping people experience joys of hearing was near and dear to her, restoring sight was precious to her, too. From her ENT experience, it was clear that community outreach must seek to serve other healthcare professionals and their patients. By practicing The Golden Rule, favorable perceptions on the ethical continuum would be fostered. As the $alesy vs. Educational Ruler reminds us, it is imperative for the clinician to strive to focus on educating our patients on the benefits of treating hearing loss. That is, the sale of our treatment occurs after we have thoroughly educated patients on their condition and why it should be treated.
By reviewing the medical system’s list and asking her own patients who provided their vision care, Janet identified multiple Ophthalmologists and Optometrists in close proximity. Just as helping people experience joys of hearing was near and dear to her, restoring sight was precious to her, too. From her ENT experience, it was clear that community outreach must seek to serve other healthcare professionals and their patients. By practicing The Golden Rule, favorable perceptions on the ethical continuum would be fostered. As the $alesy vs. Educational Ruler reminds us, it is imperative for the clinician to strive to focus on educating our patients on the benefits of treating hearing loss. That is, the sale of our treatment occurs after we have thoroughly educated patients on their condition and why it should be treated.
With a disciplined routine, she scheduled weekly times for in-person visits, often calling ahead. To boost first impressions, customized presentation folders and practice brochures would complement educational handouts. As introductory interactions were envisioned and talking points documented, she assertively prepared to discuss mutually beneficial relationships. Amid meticulous planning for January’s dual sensory loss focus, pragmatic modeling took shape for subsequent months. Step by step, change for the better.
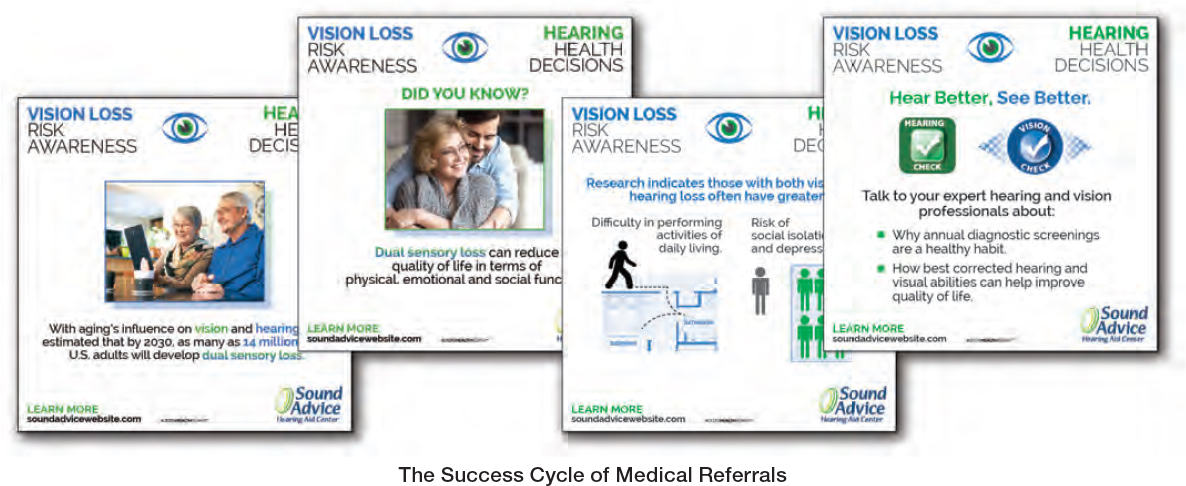
To capitalize upon In Practice and In Community programs, Online initiatives would promote Hometown Audiology’s brand, easy access, and culture. A feature-rich website would showcase her unique practice story, service lines and educational content. Monthly E-Newsletters would efficiently stay in touch with patient database, keeping comorbidity awareness top of mind and eliciting valuable response data. From what she heard, there were nifty ways to utilize this engagement tracking for outbound microtargeting purposes. In the social realm, her Facebook page prepared to feature Wellness Wednesdays, syncing with monthly topics, starting with this Vision Loss quartet:
On purpose, Hometown Audiology’s Omni-Channel comorbidity education platform would showcase audiology’s vital role in accomplishing Whole Person Care objectives. At the October medical system meeting when Janet updated peers on launch plans, feedback was exceedingly positive, including inquiries about arranging meetings to discuss ideal referral processes. With opening day imminent, Dr. Carter congratulated Janet, saying he was sure they had made an excellent decision.
Executing the Plan
Hometown Audiology’s long-awaited grand opening was festive with uplifting support from family, friends, healthcare colleagues and eager patients. While the entrepreneurial roller coaster was challenging, this high point delighted. As guests toured her clinical space, it was evident that patients’ journeys would be educationally focused on pathways to making well-informed decisions. Intuitive in nature, eye-catching canvas artwork and informative handouts were clearly seen as indispensable tools in encouraging explanatory dialogue. As expected, dozens of attendees expressed surprise at realizing hearing loss related to so many common medical conditions, clearly indicative of community awareness needs. In a significant development, multiple physicians invited her to visit their practice and discuss collaborative presentations at upcoming health fairs.
With Thanksgiving and the holiday season coming soon, her appointment schedule filled rapidly. After extensive time invested in designing her thoughtful clinical flow, it was exciting to see patients experience it and stimulate engaging quality of life conversations. Caring was sharing and research-based educational content was the center of attention, not technical jargon. With subject matter expertise gaining confidence, treatment plan discussions were naturally easier and more effective.
As clinical visits and time management challenges grew, Janet diligently blocked out time for weekly physician visits. In preparation, by reviewing their websites, useful insights were readily accessible. From contact names and areas of clinical interest, practice insights were gleaned. From experience, she knew initial engagement in a high-integrity manner was decisive, whether with receptionist, practice administrator, clinical staff or doctors themselves. Focal points included:
- Convenient patient access
- Research-based comorbidity education
- Expert care with personalized solutions
- Easy referral process
- Thorough and timely patient reports
Also important, albeit more subtle, was discussing health literacy goals and disparities, especially that patients with improved hearing acuity could communicate more effectively with all medical providers.
Janet’s presentation folders featured educational information tailored for recipients. As examples, diabetes handouts for endocrinologists, dual sensory loss for ophthalmologists, dementia for geriatricians and ototoxicity for oncologists. When conversations delved into research-based educational content, her distinguished practice philosophy was apparent. Since there had not been a trusted audiologist to refer to locally, she perceived many patients’ needs had gone unmet or they reported back unpleasant feedback from salesy encounters with the big city’s aggressive outlets. Many healthcare colleagues who tried to cope with hearing challenged folks in their care, were relieved to refer those in need.
Being respectful of time invested, at the conclusion of initial visits, collectively useful action steps were decided. From follow up meetings with staff, educational material provision or community health events, cooperative pathways were detailed and documented. While somewhat apprehensive prior to interactions, it was rewarding to know whole person care guiding principles were a healthy impetus and conversational tailwind. With autonomy to be responsive, innovative ideas could be acted on in days or weeks, not months or years. In preparation for the holiday season, Janet co-hosted a Super Seniors “Sights and Sounds” educational event with a popular optometric practice. Together, they recognized the importance of raising awareness those not seeing or hearing their best often struggled with activities of daily living. The healthy reactions to engaging presentations were noteworthy as attendees welcomed learning about dual sensory loss topics simultaneously. Quality of life chords were struck, and a valuable community education model took shape, one which would be applicable to various medical disciplines.
The holiday season flew by quickly, as Janet’s patients delighted in the Joys of Hearing. She cherished Hometown Audiology’s strong start and all those who supported her professional growth, from formal training to ENT practice, along with influential colleagues, family, and friends. As a wise mentor advised, when people believe in you, do all you can to prove them right and then, do your best to empower others with similar goals.
With 2023 an exciting destination, Janet conscientiously got strategic thoughts on paper. In doing so, she considered processes involved in guiding her trusting patients to make healthy decisions which led to positively reinforcing cycles. With analogies useful, how should grassroots educational marketing plans be “Diagnosed and Treated” in terms of identifiable steps, ideally sequenced. After introspection and iterative series of sketches, the visual, Success Cycles Matters was created to illustrate how the entire educational marketing strategy fits together.
Throughout her first full year, practice growth trends exceeded expectations. In Practice, wellness referrals flourished as educated patients advocated with others in their circle of life. In Community, one trusting relationship led to another as local healthcare providers embraced her expertise, appreciated her personalized reports, and consistently listened to enthusiastic testimonials from those entrusted in her care. Online, Hometown Audiology’s social media presence expanded. As her patient database grew, an Educate Well Monthly E-Newsletters was launched. With an informative mix of content, engagement measures were exceptionally high, delivering valuable response data to thoughtfully segment for timely nurturing. With rapidly expanding numbers of views and clicks, this was a logical way to grow her practice from the inside out and friendly phone calls were pleasant surprises.
As audiology colleagues inquired about Janet’s entrepreneurial journey, there was keen interest in methods to so deftly navigate her successful career transition. Looking back, although explaining her practice development sequence sounded logical, she stressed how necessary it had been to not let pursuit of perfection get in the way of progress. When counseling others considering starting their own practices, she candidly described typical challenges, growth opportunities and bedrock guiding principles. Chief among them was the core belief that educationally empowering patients with trusted advice was an ethical way to achieve best outcomes. While intuitively known that wellness and physician referrals were essential growth drivers, in reality, virtuous cycles resulted when folks who were happy to hear spread praise with family, friends, and other healthcare providers. She was a subject matter expert on the public health benefits of interdisciplinary care, who constantly boosted her knowledge on hearing-related comorbidities.
One day, after receiving heartwarming feedback from patients whose lives were changed for good, Janet treasured a reflective moment. Deep down, she knew Grandpa Dave would be proud of how, in trustworthy ways, she was doing her part to Elevate the Profession. With the utmost humility, as an educational curator, she had seized the day and hopefully others would be inspired to do so as well. Carpe’ Diem! ■
References
- Nair EL, Cienkowski KM. The impact of health literacy on patient understanding of counseling and education materials. Int J Audiol. 2010 Feb;49(2):71-5. doi: 10.3109/14992020903280161. PMID: 20151879.
- World Health Organization. Improving Health Literacy webpage. Accessed at the following location: https://www.who.int/activities/improving-health-literacy#:~:text=. on September 12, 2022.
- National Institute of Health (NIH). National Eye Institute. Glaucoma Awareness Month Resources. Accessed at the following location: https://www.nei.nih.gov/learn-about-eye-health/outreach-campaigns-and-resources/glaucoma-resources/glaucoma-awareness-month on September 12, 2022.
